If you're reading this, chances are you're seeking answers to the relentless pelvic pain that's affecting your quality of life. You're not alone; countless women are in the same boat, often feeling isolated and overwhelmed. This guide is your lifeline. It's designed to empower you with knowledge, from pinpointing the root causes to navigating the maze of diagnostic tests and treatment options. We aim to be your trusted companion on this journey, helping you reclaim your life from the clutches of pain.
What Is Pelvic Pain in Women?
Pelvic pain in women is a complex and often misunderstood condition that affects the lower abdomen or pelvis. However, it's not just a physical symptom but a multifaceted issue that can significantly impact various aspects of life, from emotional well-being to daily activities.
Nearly one in seven women experience chronic pelvic pain. Yet, despite its prevalence, it remains a largely under-discussed and under-diagnosed issue. This lack of awareness exacerbates the suffering, affecting not just the individual but also relationships, careers, and overall quality of life.
Some of the typical ways the pain can manifest are:
- A dull ache that lingers
- Sharp, debilitating cramps that come and go
- Acute pain that appears suddenly and severely
- Chronic discomfort that persists over a long period
What Causes Pelvic Pain in Women?
Understanding the root causes of pelvic pain in women is essential for effective diagnosis and treatment. The condition is often a complex interplay of various factors – physical, emotional, and even environmental. Here's a deeper look into some of the most common causes:
Endometriosis
Endometriosis occurs when tissue resembling the uterine lining grows outside the uterus, often affecting the ovaries, fallopian tubes, or even the intestines. This can result in intense discomfort, particularly during menstruation, and may lead to complications like infertility. Furthermore, it may also occur at different stages of the menstrual cycle and could be associated with gastrointestinal issues.
Pelvic Pain During and After Pregnancy
During pregnancy, discomfort can arise from the stretching and loosening of ligaments and the added weight of the baby. This is often felt as a dull ache or sharp, shooting pains. Postpartum, some women may experience persistent distress due to complications like pelvic girdle pain or issues related to cesarean section recovery.
Muscle Spasms
Muscle spasms involve involuntary contractions of the pelvic floor muscles. These can result in sharp, stabbing pain that may be triggered by certain movements or activities, making it challenging to predict or manage without medical intervention.
Psychological Factors
Stress, anxiety, and depression can have a tangible impact on pelvic pain. Such a state of mind can exacerbate physical symptoms, creating a vicious cycle where mental distress intensifies the discomfort, which in turn worsens the emotional condition.
Interstitial Cystitis
Interstitial cystitis, also known as painful bladder syndrome, can cause persistent pressure and discomfort in the pelvic region. Symptoms often mimic those of a urinary tract infection (UTI) but last much longer and may fluctuate in intensity.
Gastrointestinal Issues
Certain gastrointestinal conditions, like irritable bowel syndrome (IBS), can manifest as pelvic pain. This is often accompanied by other symptoms like bloating, diarrhea, or constipation, making it crucial to consider gastrointestinal health when diagnosing the discomfort.
Pelvic Inflammatory Disease (PID)
PID is an infection that targets the female reproductive organs, commonly stemming from sexually transmitted bacteria like chlamydia or gonorrhea. The condition can cause sharp pelvic pain and irregular menstrual cycles and, if left untreated, can escalate to infertility or ectopic pregnancy.
Ectopic Pregnancy
An ectopic pregnancy is a life-threatening condition where a fertilized egg implants outside the uterus, usually in a fallopian tube. This can lead to severe discomfort, often accompanied by symptoms like vaginal bleeding and shoulder pain.
Urinary Tract Infections
UTIs are bacterial infections affecting the urinary system, which includes the bladder, kidneys, and urethra. They can cause symptoms like a burning sensation during urination, frequent urges to urinate, and lower abdominal or pelvic pain. UTIs are more common in women and can often be treated effectively with antibiotics.
6 Treatments for Pelvic Pain in Women
The treatment for pelvic pain varies depending on the underlying cause, and it often involves a combination of medical and lifestyle interventions. Here are some common treatment options:
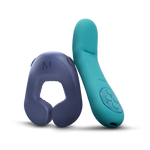
1. Sexual Wellness Devices

Step into a transformative realm of health and sexual wellness with Crescendo 2, an FDA-approved device that's redefining the landscape of pelvic pain management. Clinically proven to alleviate the challenges of genito pelvic pain disorder and arousal disorder, Crescendo 2 is more than just a wellness tool; it's a lifeline for those grappling with symptoms from childbirth, menopause, and other conditions that affect pelvic health.
What sets Crescendo 2 apart is its innate adaptability. Designed to mold to your unique body shape, it ensures targeted relief right where you need it most. This is complemented by the device's ability to deliver medical-frequency vibrations with pinpoint accuracy, thanks to its six strategically positioned motors.
But the customization doesn't stop there. With the intuitive smart app, you can fine-tune each motor's pattern and intensity level, allowing you to craft a tailored healing journey that aligns with your specific needs and preferences. Moreover, quality and safety are non-negotiable, which is why Crescendo 2 is crafted from water-resistant, medical-grade silicone. It's also USB rechargeable, ensuring that both convenience and safety are integral parts of your experience.
Beyond its impressive array of therapeutic benefits, Crescendo 2 serves as a gateway to pleasure. It adds a new, enriching dimension to your wellness journey, allowing you to explore and embrace a fuller, more vibrant life.
Experience the transformative power of Crescendo 2 today and reclaim your life.
2. Physical Therapy

Physical therapy is an invaluable component of a comprehensive approach to managing symptoms. Specialized exercises, often guided by a certified pelvic floor physical therapist, focus on strengthening the pelvic muscles and improving posture to alleviate discomfort.
Techniques such as manual therapy and biofeedback can also be employed to relax tense muscles and improve bodily awareness. The goal is not just symptom relief but also empowering you with the tools to manage your health long-term. With consistent physical therapy, many individuals experience significant improvements, making it a highly recommended treatment option for various types of pelvic pain.
3. Cognitive Behavioral Therapy (CBT)

Cognitive Behavioral Therapy (CBT) is increasingly recognized as an effective treatment for pelvic pain, particularly when the discomfort is linked to stress, anxiety, or past trauma. This psychological approach aims to identify and alter thought patterns and behaviors that contribute to pain.
Through a series of guided sessions, individuals learn coping mechanisms, relaxation techniques, and strategies to manage triggers. By addressing the mental and emotional aspects of the discomfort, CBT offers a holistic approach that complements medical treatments. It empowers individuals to take control of their symptoms, providing both immediate relief and long-term management strategies.
4. Acupuncture

Acupuncture, a crucial part of traditional Chinese medicine, is gaining traction as a viable treatment option for pelvic pain. By inserting fine needles into specific points on the body, acupuncture aims to balance the flow of energy or "qi," thereby promoting natural healing and improving bodily functions.
One of the key advantages of acupuncture is that it offers a non-pharmacological option for pain relief. This is particularly beneficial for individuals who may be sensitive to medications or are looking for a more natural approach to treatment. Moreover, acupuncture is generally considered safe when performed by qualified practitioners, with minimal side effects such as temporary soreness or bruising at the needle sites.
5. Dietary Changes

Modifying your diet can be a powerful way to manage discomfort, especially when inflammation is a contributing factor. To this end, a diet rich in anti-inflammatory foods such as fruits, vegetables, and omega-3 fatty acids can help alleviate symptoms. Eliminating or reducing foods that trigger inflammation, such as processed foods, sugars, and certain types of fats, can also bring relief.
Additionally, some individuals may find that specific dietary protocols, like the Low FODMAP diet, can be particularly effective for conditions like IBS, which often coexists with pelvic pain. Simply, by focusing on nourishment that supports pelvic health, dietary changes offer a non-invasive treatment option that can significantly improve quality of life.
6. Hormone Therapy

Hormone therapy is often considered for conditions like endometriosis or hormonal imbalances that contribute to symptoms. By administering hormones such as estrogen or progestin, this treatment aims to regulate menstrual cycles, reduce the growth of abnormal tissue, and alleviate pain.
Fortunately, hormone therapy can come in various forms, including oral contraceptives, hormone-releasing IUDs, or even injections. While these treatments can be highly effective, consulting a healthcare provider for a thorough evaluation is crucial. This is because the treatment can carry side effects and may not be suitable for everyone.
Conclusion
Pelvic discomfort in women is a complex problem that necessitates an all-encompassing strategy for both diagnosis and management. Understanding the underlying causes and available treatment options is the first step in managing this condition effectively. Don't let pelvic pain control your life; take action today to reclaim your well-being.